A lot of us think of digestion as something that either works or doesn’t, but the truth is more interesting: digestion is an evolving story that changes as we move through childhood, adolescence, adulthood, midlife, and our later years. This article walks you through those changes step by step, explains why they happen, and gives practical, age-appropriate strategies to support digestion and overall wellness. I’ll keep things conversational and clear, and I’ll give you checklists, a helpful table, and real-world tips you can use right away.
Step 1: The Basics — What Digestion Does and Why Age Matters
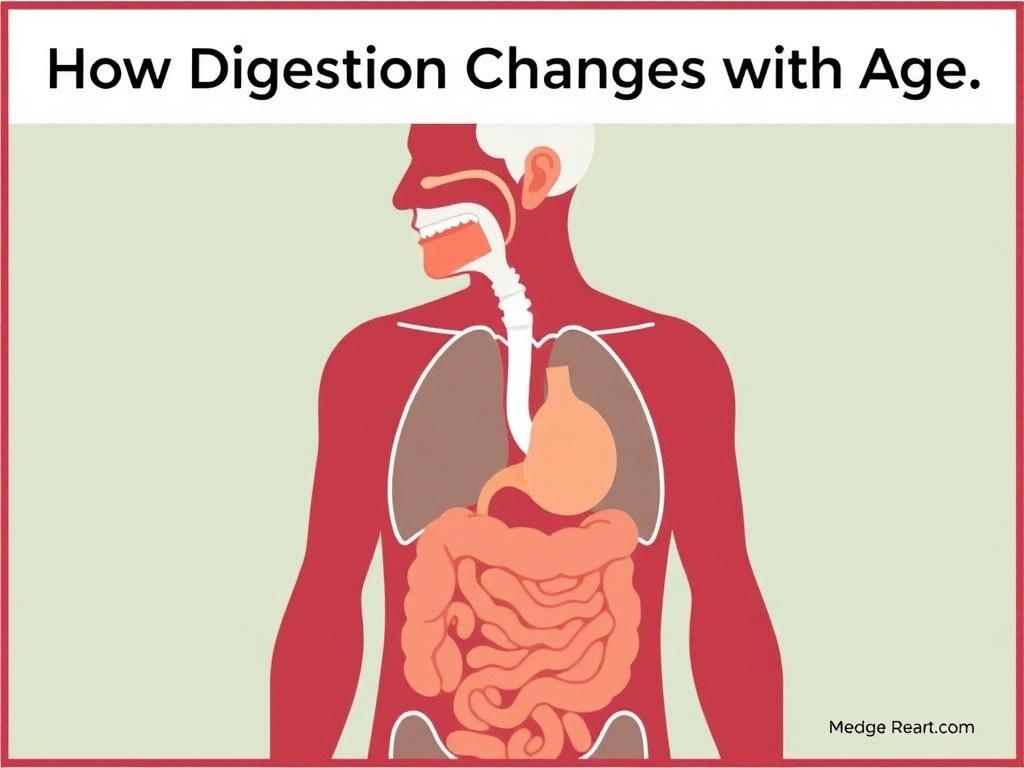
Think of digestion as an assembly line that starts when food hits your mouth and ends when your body has extracted nutrients and gotten rid of waste. Along this line, many processes must work smoothly: chewing, swallowing, stomach acid breaking down food, enzymes from the pancreas and gut working, bile emulsifying fats, the small intestine absorbing nutrients, and the colon forming and eliminating stool. Every stage depends on muscles, nerves, glands, microbiota, and a steady supply of fluids.
As we age, every one of those players changes in subtle or obvious ways. Some of the changes are predictable and natural; others are consequences of lifestyle, medications, or illnesses we pick up over the years. What matters most is understanding which changes are expected and which warrant a conversation with your healthcare provider.
Step 2: How Digestion Develops — Childhood and Adolescence
Your digestive system does a lot of growing in childhood. Babies and young children gradually develop enzyme systems and gut flora, and by adolescence the system is usually mature. Still, childhood is the time when foundational habits form — what we eat, how we chew, and even how we handle stress.
Infancy and Early Childhood
In the first months and years of life, digestion is still learning to be efficient. Breast milk or formula supplies easily digested nutrition. As solids are introduced, infants learn to chew, and their gut microbiome diversifies.
- Enzyme levels: Immature but rapidly maturing; lactase is high in infancy and may decline later for some people.
- Immune learning: The gut-associated immune system is developing, which helps determine future reactions to foods.
- Microbiome: Rapid shifts as babies encounter new foods and environments.
School Age to Teenagers
By school age, digestion is largely adult-like, but appetite, metabolism, and hormones change notably in adolescence. Teenagers often experience irregular eating patterns, fast food or processed diets, and stress, all of which affect digestion.
- Increased caloric needs and variable appetite.
- Acid reflux may start in some teens, especially with obesity or hiatal hernia.
- Constipation can be common due to low fiber intake, dehydration, or behavioral withholding.
Step 3: Adulthood — Prime Time and New Challenges
Adult digestion generally runs smoothly, but lifestyle begins to play a larger role. Stressful jobs, alcohol, caffeine, irregular meals, low activity, and weight changes all shape gut health. Hormonal changes—especially for women during pregnancy or with fluctuating cycles—affect motility and reflux.
Common Adult Digestive Patterns
- Faster recovery from minor digestive upsets than in older age, typically.
- Higher risk behaviors (smoking, excess alcohol) can cause gastritis, reflux, and liver issues.
- Emergence of functional GI disorders, such as irritable bowel syndrome (IBS), often in the 20s-40s.
When to Pay Attention
If symptoms like persistent heartburn, unintended weight loss, blood in stool, difficulty swallowing, or severe abdominal pain appear, adults should see a healthcare provider promptly—these could signal conditions requiring testing or treatment.
Step 4: Midlife Changes — Hormones, Metabolism, and Emerging Issues
Midlife often brings slower metabolism, changes in body composition, and for many people, hormonal shifts like perimenopause. These changes can influence digestion in several ways.
Motility and Transit Time
Aging tends to slow gut motility a bit. That means food can move more slowly through the digestive tract, increasing the risk of constipation. This change is gradual and may be compounded by less physical activity, medications, and lower fluid intake.
Acid, Enzymes, and Absorption
Stomach acid levels can fall with age or with medication use (e.g., long-term proton pump inhibitors). Lower acid may impair digestion of proteins and absorption of nutrients like vitamin B12, iron, calcium, and magnesium. Pancreatic enzyme production may remain adequate for many people, but illnesses or chronic pancreatitis can reduce enzyme output and lead to malabsorption.
The Gut Microbiome
Midlife brings shifts in the microbial community in your gut. Diet, antibiotics, and lifestyle change the microbiome composition, which can affect inflammation, metabolism, and immune function. A less diverse microbiome is often associated with poorer digestive outcomes.
Step 5: Later Life — What to Expect for Older Adults
As we enter older adulthood, more noticeable and frequent digestive changes can appear. Some are natural, others are due to cumulative exposures, medicines, dental problems, or chronic diseases.
Key Changes in Older Age
- Reduced stomach acid (hypochlorhydria) for some people, which can affect protein digestion and nutrient absorption.
- Slower intestinal transit and a higher risk of constipation.
- Increased risk of gastroesophageal reflux disease (GERD) or complications from chronic reflux.
- Higher prevalence of diverticulosis and associated diverticulitis in some populations.
- Altered taste and smell, dental issues, and swallowing problems (dysphagia).
- Changes in the gut microbiome toward less diversity.
Medications: A Big Part of the Picture
Older adults typically take more medications, many of which affect digestion: opioids slow motility, anticholinergics cause dry mouth and delayed gastric emptying, calcium supplements and iron can cause constipation, and antibiotics can disrupt the microbiome. Long-standing use of acid-lowering drugs can impact nutrient absorption. Medication review with a clinician is essential to manage digestive side effects.
Step 6: Specific Digestive Conditions That Increase with Age
Certain digestive disorders become more common or change in presentation as we age. Recognizing these early helps with better outcomes.
Common Age-Related Conditions
- Constipation — more common due to slower transit, lower activity, dehydration, and medications.
- Diverticulosis and diverticulitis — small pouches in the colon increase with age; when inflamed they cause pain and fever.
- Colon polyps and cancer — risk increases with age; screening is vital.
- Gastroesophageal reflux disease (GERD) — may persist or worsen, sometimes presenting with atypical symptoms like coughing or chest pain.
- Swallowing problems (dysphagia) — can be caused by neurological conditions, muscle weakness, or structural problems.
- Malabsorption and vitamin deficiencies — B12 deficiency becomes more likely with reduced stomach acid or after certain surgeries.
- Gallstones — prevalence rises with age and can cause sudden biliary colic or cholecystitis.
Step 7: Nutrient Absorption — What Changes and Why It Matters
As digestion changes, absorption of key nutrients can be affected. This has real health implications for energy, bone health, cognition, and immunity.
Vitamins and Minerals of Concern
| Nutrient | Why It Can Decline with Age | Potential Consequences |
|---|---|---|
| Vitamin B12 | Reduced stomach acid and intrinsic factor, or use of acid-suppressing drugs, can impair absorption. | Anemia, fatigue, neuropathy, cognitive issues. |
| Iron | Lower stomach acid reduces iron absorption; blood loss also becomes a concern. | Anemia, weakness, reduced exercise tolerance. |
| Calcium and Vitamin D | Absorption may decrease with age; dietary intake often falls as well. | Bone loss, increased fracture risk. |
| Protein | Lower appetite, chewing problems, and slower digestion may reduce intake. | Loss of muscle mass (sarcopenia), weaker immunity, slower recovery from illness. |
| Fat-soluble vitamins (A, D, E, K) | Conditions that impair fat absorption (e.g., pancreas, bile issues) reduce uptake. | Varied effects including bone and immune issues. |
Practical Takeaways on Nutrition
Good nutrition throughout life helps mitigate age-related declines. Focus on adequate protein, fiber, calcium, vitamin D, and foods rich in B vitamins. If you have symptoms like chronic diarrhea, unintended weight loss, or signs of deficiency, talk to your healthcare provider about testing and possible supplements.
Step 8: The Gut Microbiome and Aging
Your gut hosts trillions of microbes that help digest food, regulate the immune system, and communicate with the brain. The microbiome tends to lose diversity with age, and that can affect digestion and inflammation.
Factors That Influence Microbiome Health
- Diet: Fiber-rich, varied diets support diversity. Processed foods and low-fiber diets reduce it.
- Antibiotics: These can cause long-lasting shifts if used repeatedly or indiscriminately.
- Medications: Many drugs (including proton pump inhibitors and metformin) affect microbial composition.
- Illness and hospitalization: These can reduce resilience of the microbiome.
- Probiotics and prebiotics: May help restore balance in certain situations.
Tips to Support a Healthy Microbiome
- Eat a diversified plant-rich diet: fruits, vegetables, whole grains, legumes, nuts, and seeds.
- Limit highly processed foods and excessive sugar.
- Use antibiotics only when necessary and follow guidance on when to take probiotics (ask your doctor).
- Consider fermented foods like yogurt, kefir, sauerkraut, and kimchi if tolerated.
- Stay physically active and manage stress—both help maintain microbiome diversity.
Step 9: Lifestyle Strategies to Support Digestion at Every Age
Small lifestyle changes can make a big difference. Here are practical, age-appropriate strategies.
Daily Habits for Better Digestion
- Stay hydrated: Water helps keep stool soft and supports enzymatic reactions.
- Prioritize fiber: Strive for whole-food sources of soluble and insoluble fiber to support regularity.
- Move regularly: Exercise stimulates bowel motility and helps manage weight.
- Eat mindfully: Chew well, eat at a relaxed pace, and don’t eat right before bed if you’re prone to reflux.
- Monitor medicine effects: Ask your provider about digestive side effects and alternatives if needed.
- Oral health: Healthy teeth and dentures or dental care support proper chewing and digestion.
Meal Ideas by Life Stage
| Life Stage | Meal Focus | Example Meals |
|---|---|---|
| Children | Balanced nutrients, texture variety, iron-rich foods for toddlers | Oatmeal with mashed banana and milk; chicken and sweet potato; yogurt with fruit. |
| Young Adults | Energy-dense, nutrient-packed meals supporting activity and learning | Stir-fry with tofu and mixed veggies over brown rice; lentil soup and salad. |
| Midlife | Maintain muscle and bone health; fiber to prevent constipation | Grilled salmon, quinoa, roasted vegetables; Greek yogurt with walnuts and berries. |
| Older Adults | Higher protein, easy-to-chew foods, foods rich in B12 and calcium | Soft-cooked eggs, mashed avocado toast, vegetable stew with beans, fortified cereals. |
Step 10: When to See a Doctor — Warning Signs and Screening
Some symptoms are part of normal aging or temporary upset, but others require prompt attention. Don’t hesitate to seek medical care for:
- Unexplained weight loss
- Persistent or worsening abdominal pain
- Bloody stool or black tarry stool
- Difficulty swallowing
- New onset of severe constipation or diarrhea lasting weeks
- Persistent vomiting or inability to keep fluids down
Screening and Tests That Matter
— Colonoscopy: Recommended starting at age 45–50 for average-risk adults, earlier for higher risk or symptoms, and repeated at intervals based on findings. Screening prevents colorectal cancer by finding and removing polyps.
— Upper endoscopy: Useful for persistent reflux, dysphagia, or upper GI bleeding.
— Blood tests: Check for anemia, vitamin B12, iron, and metabolic abnormalities.
— Breath and stool tests: Diagnose infections (like H. pylori), small intestinal bacterial overgrowth (SIBO), or malabsorption.
— Imaging: Ultrasound or CT for gallstones, pancreatitis, or structural problems.
Step 11: Managing Specific Problems — Practical Approaches
Here are approachable ways to manage common concerns that change with age.
Constipation
- Increase fiber gradually (fruits, vegetables, whole grains) and fluids to prevent gas and bloating.
- Regular physical activity helps stimulate bowel movements.
- Establish a bathroom routine; try going 15–30 minutes after meals to use the gastrocolic reflex.
- Use stool softeners, osmotic laxatives, or stimulants under the guidance of a clinician for short-term help; long-term reliance should be evaluated.
Reflux and Heartburn
- Eat smaller, more frequent meals and avoid eating within 2–3 hours of lying down.
- Avoid trigger foods (spicy, fatty, chocolate, caffeine, alcohol) and tight clothing at the waist.
- Lose weight if overweight and elevate the head of the bed if nighttime reflux occurs.
- Discuss medication needs with your provider—long-term acid suppression has pros and cons.
Swallowing Difficulties
Nutrient Deficiencies
Step 12: Surgeries and Structural Changes That Affect Digestion
Some surgeries and age-related structural changes alter digestion permanently. Examples include gastric bypass, fundoplication, gallbladder removal, and resection of bowel due to disease. Each has unique implications:
- Gastric bypass: Alters absorption and can cause dumping syndrome; requires lifelong attention to nutrition and supplements.
- Gallbladder removal: Many people adjust with few long-term issues, but some experience looser stools or changes in fat digestion.
- Bowel resections: Depending on how much is removed, malabsorption and faster transit can occur.
If you’ve had surgery, regular follow-up and nutritional monitoring are important.
Step 13: Mental Health, Stress, and the Gut-Brain Connection
The gut and brain are in constant communication. Stress, anxiety, and depression can alter motility, increase sensitivity to pain, and change the microbiome. Functional conditions like IBS often reflect an overactive gut-brain dialogue.
Ways to Support the Gut-Brain Axis
- Practice stress-reduction techniques: mindfulness, meditation, deep breathing, yoga, or counseling.
- Keep social connections and routines that reduce chronic stress.
- Consider cognitive behavioral therapy or gut-directed therapies for chronic GI symptoms; they can be highly effective.
Step 14: Supplements, Probiotics, and Over-the-Counter Aids — Use Wisely
Supplements can help but aren’t a cure-all. Probiotics may relieve certain conditions (e.g., antibiotic-associated diarrhea, irritable bowel symptoms) but results vary by strain and dose.
Rules of Thumb
- Consult a provider before starting supplements, especially if you take other medications or have chronic disease.
- Use evidence-based choices: B12 for deficiency, calcium and vitamin D for bone health, iron only for documented deficiency, and individualized probiotics when helpful.
- Avoid relying on unregulated products that promise quick fixes; quality varies widely among brands.
Step 15: Putting It All Together — A Simple, Age-Smart Plan
Here’s a practical plan you can adapt for any stage of life. Think of it as a checklist to keep your digestive system resilient.
- Eat a fiber-rich, varied diet with adequate protein.
- Stay hydrated and active every day.
- Limit highly processed foods, excessive alcohol, and smoking.
- Watch medications that affect digestion and review them regularly with your clinician.
- Get recommended screenings (colon cancer screening, dental, and age-appropriate labs).
- Listen to your body: seek help for red-flag symptoms or new, persistent issues.
- Support your microbiome with whole foods and judicious probiotic use if appropriate.
- Manage stress and sleep well—both influence digestion more than you might expect.
Sample Daily Routine for Digestive Health
- Morning: Start with a glass of water, a protein-rich breakfast, and gentle movement (a walk or stretching).
- Midday: Have a balanced lunch with whole grains, vegetables, and lean protein. Try to get up and move every hour.
- Afternoon: Snack on fruit, nuts, or yogurt. Hydrate well.
- Evening: Eat a lighter dinner earlier in the evening. Finish eating at least a couple of hours before bed.
- Night: If reflux is an issue, elevate the head of the bed and avoid late-night snacking.
Step 16: Myths and Misconceptions about Aging and Digestion
Let’s clear up a few common misunderstandings.
Myth: Digestive problems are just “part of getting old” and nothing can be done.
Truth: While some changes are expected, many problems are treatable or manageable with diet, lifestyle, and medical care.
Myth: Everyone needs to take a probiotic or digestive enzyme as they age.
Truth: Not necessarily. Some people benefit, but many don’t need routine supplementation. Use them when evidence suggests benefit for a specific problem.
Myth: Heartburn means you must take acid blockers forever.
Truth: Acid blockers are effective for many, but lifestyle changes, weight loss, and targeted therapies may reduce reliance. Long-term medication needs should be discussed with a clinician.
Step 17: Practical Tools — When and How to Track Symptoms
Tracking helps you and your healthcare provider identify patterns and triggers.
How to Keep a Simple Digestive Diary
- Record what you eat and drink and the time you ate.
- Note symptoms, their severity, and timing relative to meals.
- Record bowel movement frequency and consistency (consider using a simple scale like Bristol Stool Chart descriptions).
- Note medications, stress levels, sleep quality, and physical activity.
This information often reveals connections you might not notice otherwise, such as particular foods or late-night meals triggering reflux.
Step 18: Caring for Loved Ones — Digestive Changes in Older Relatives
If you care for an older relative, digestion is a common area of concern. Watch for signs of poor intake, swallowing problems, weight loss, constipation, or dehydration.
Caregiver Tips
- Ensure meals are nutrient-dense and easy to chew when needed.
- Monitor medications that impact appetite or digestion.
- Encourage gentle activity and regular bathroom routines.
- Communicate with healthcare providers about any changes in appetite, weight, or bowel habits.
Step 19: The Future — Research and New Directions
The science of digestion and aging is evolving. Researchers are exploring how the microbiome affects aging, how personalized nutrition can optimize gut health at different life stages, and how novel therapies like fecal microbiota transplant or targeted probiotics might help in the future.
It’s an exciting time—advances may soon offer more precise ways to maintain digestive health across the lifespan.
Conclusion
Aging changes digestion in many predictable ways—slower transit, altered enzyme and acid production, shifts in the microbiome, and greater vulnerability to certain conditions—but most changes are manageable with informed lifestyle choices, regular screenings, thoughtful medication use, and timely medical care; by paying attention to diet, hydration, activity, and stress, and by working with healthcare providers when symptoms arise, you can support a healthy digestive system at every stage of life.
Читайте далее: