Endoscopy and colonoscopy are words that get tossed around in clinics, on health websites, and in conversations when someone is having unexplained stomach pain or is due for cancer screening. They sound technical and perhaps a little intimidating, but once you break them down they’re straightforward tools doctors use to see inside the digestive tract. Understanding the difference between these two procedures, why a physician might recommend one over the other, what to expect before, during and after, and how to prepare can take a lot of the mystery — and fear — out of the experience. In this article I’ll walk you through the key differences and similarities in plain English, give practical tips, bust a few myths, and help you feel prepared and informed should you or a loved one need one of these procedures.
What is an endoscopy? What is a colonoscopy?
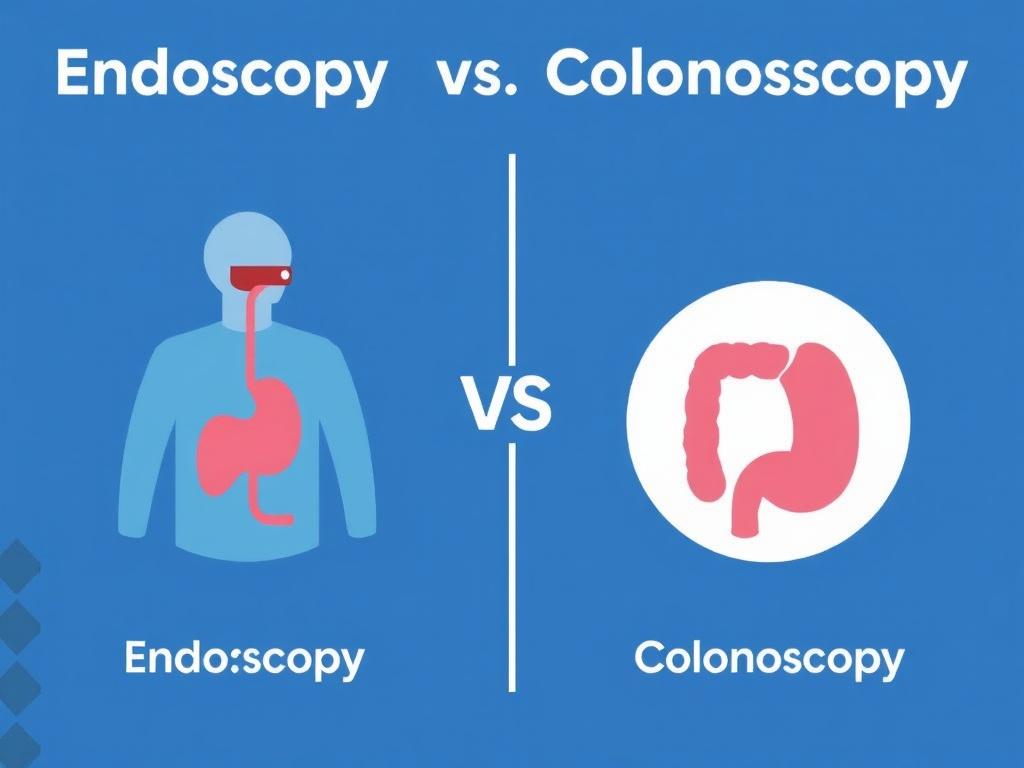
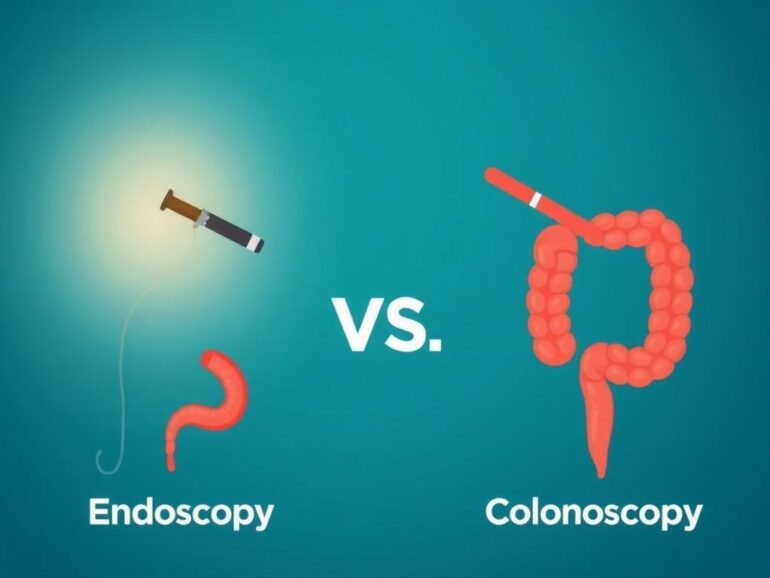
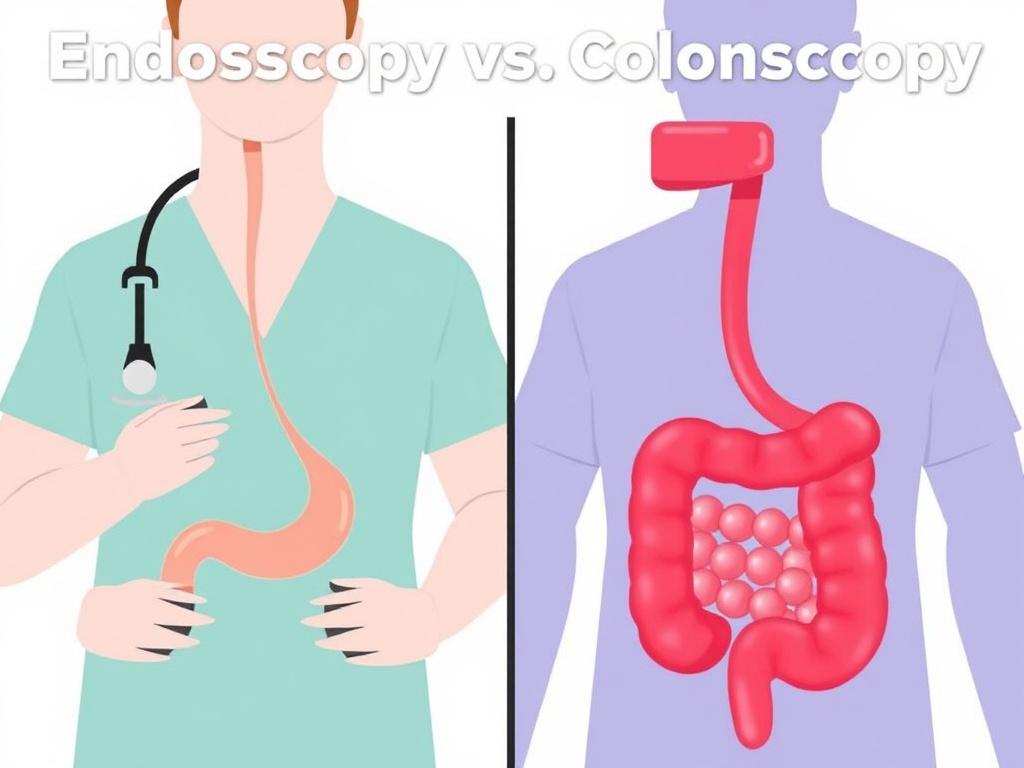
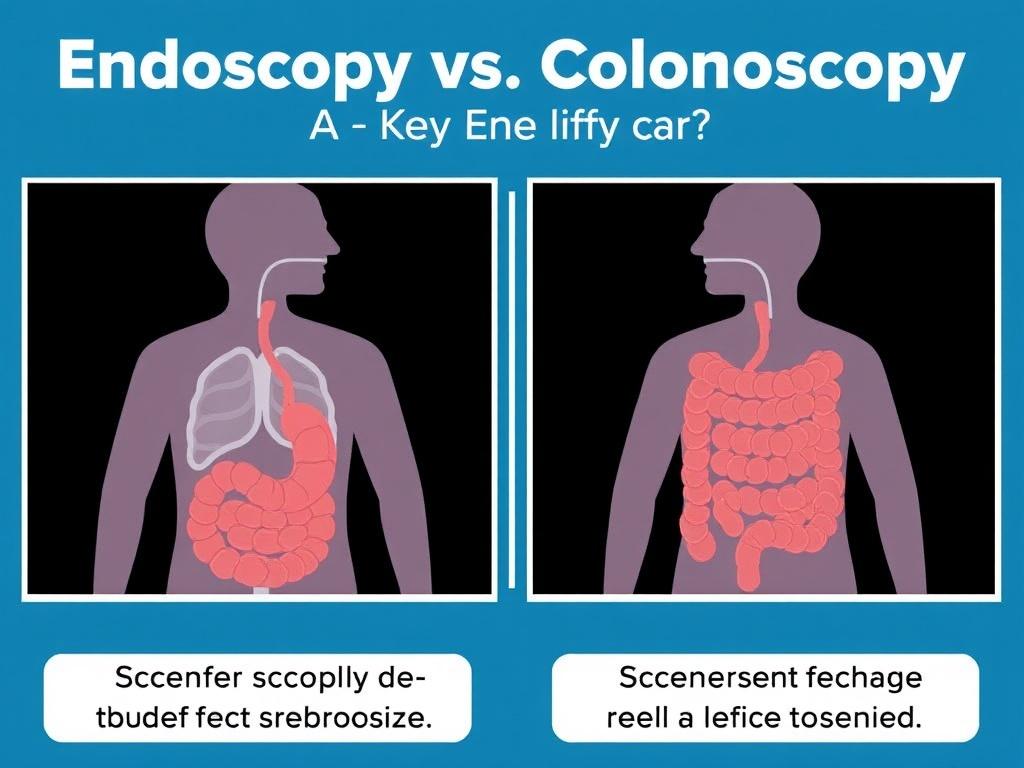
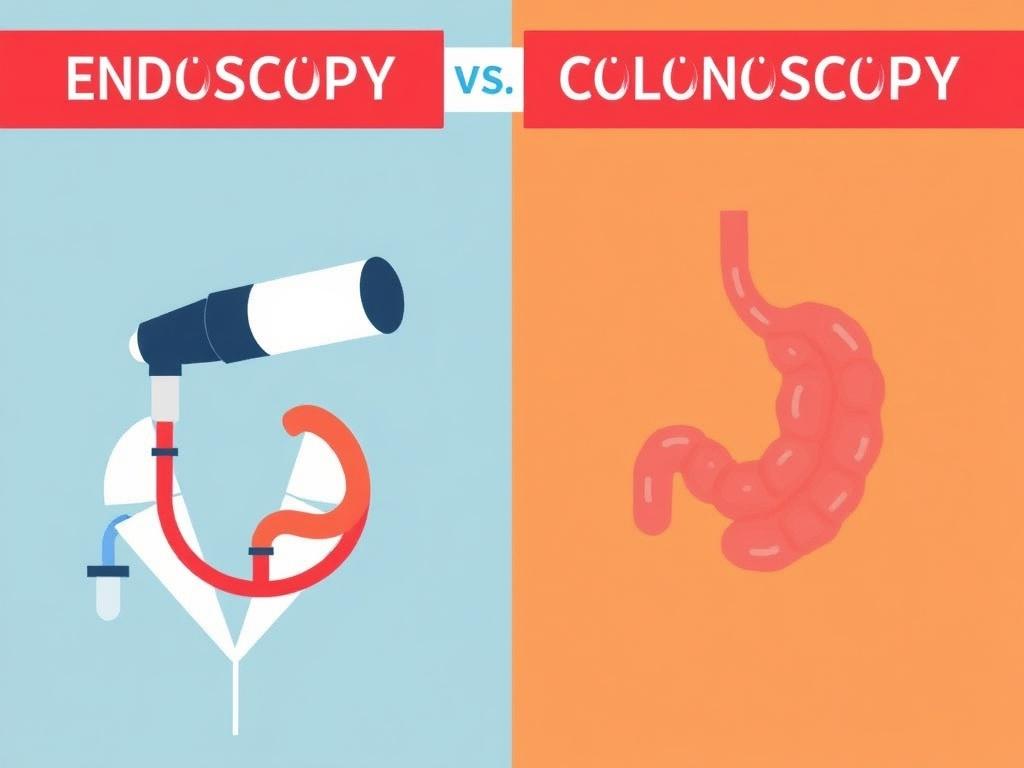
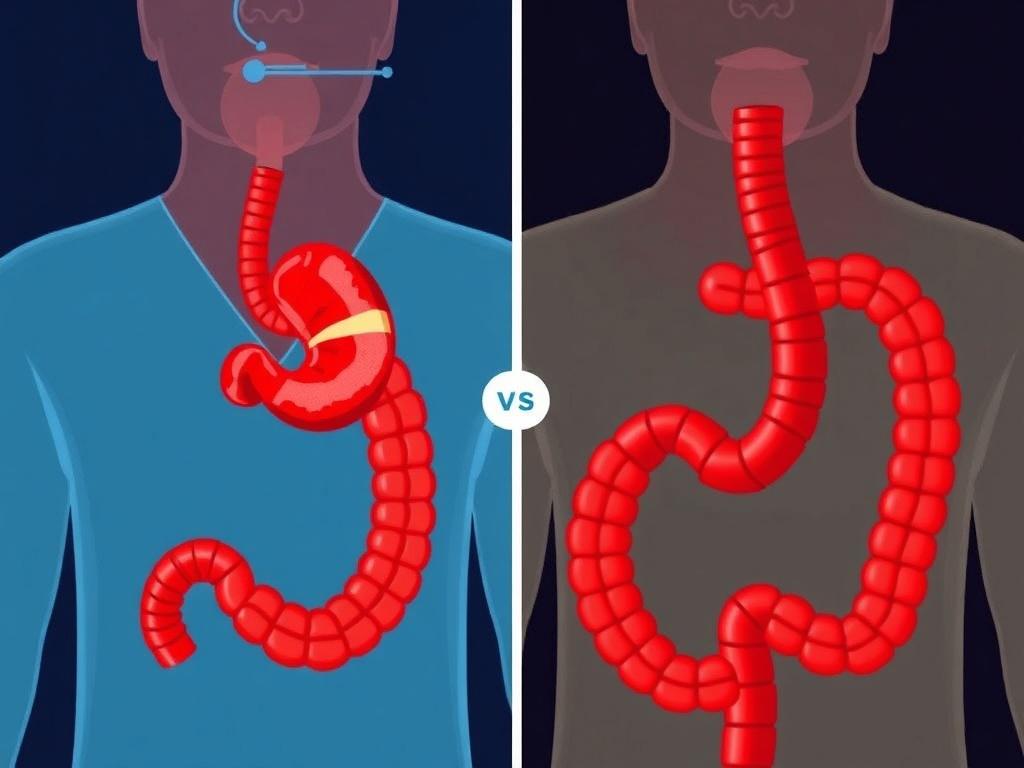
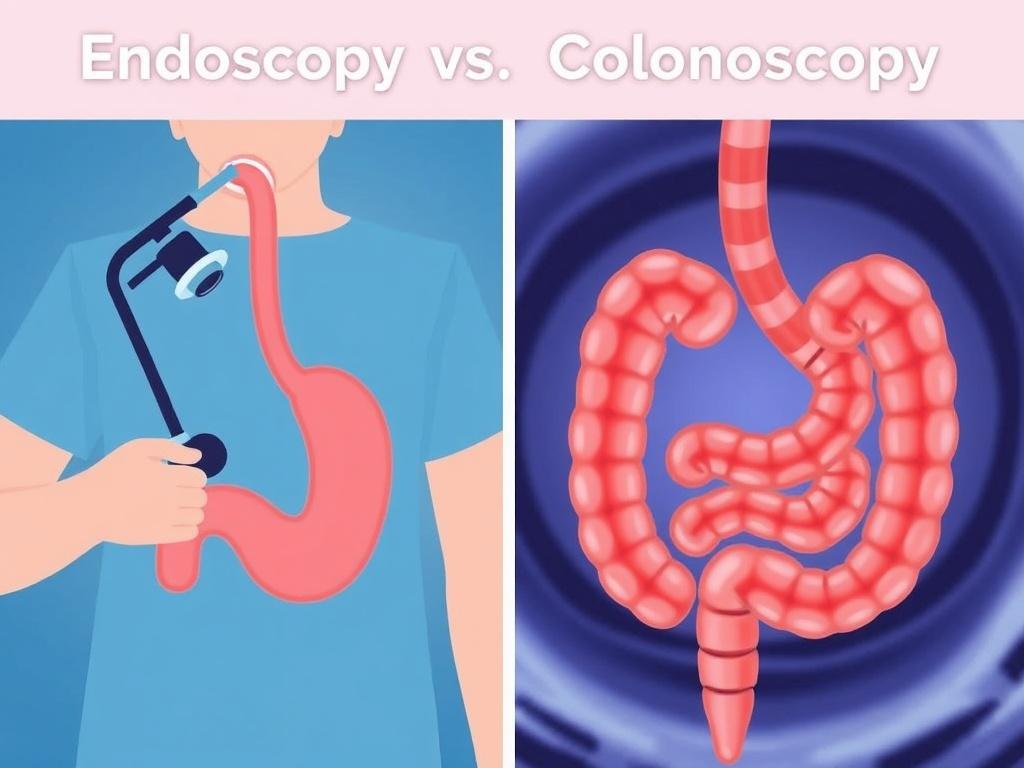
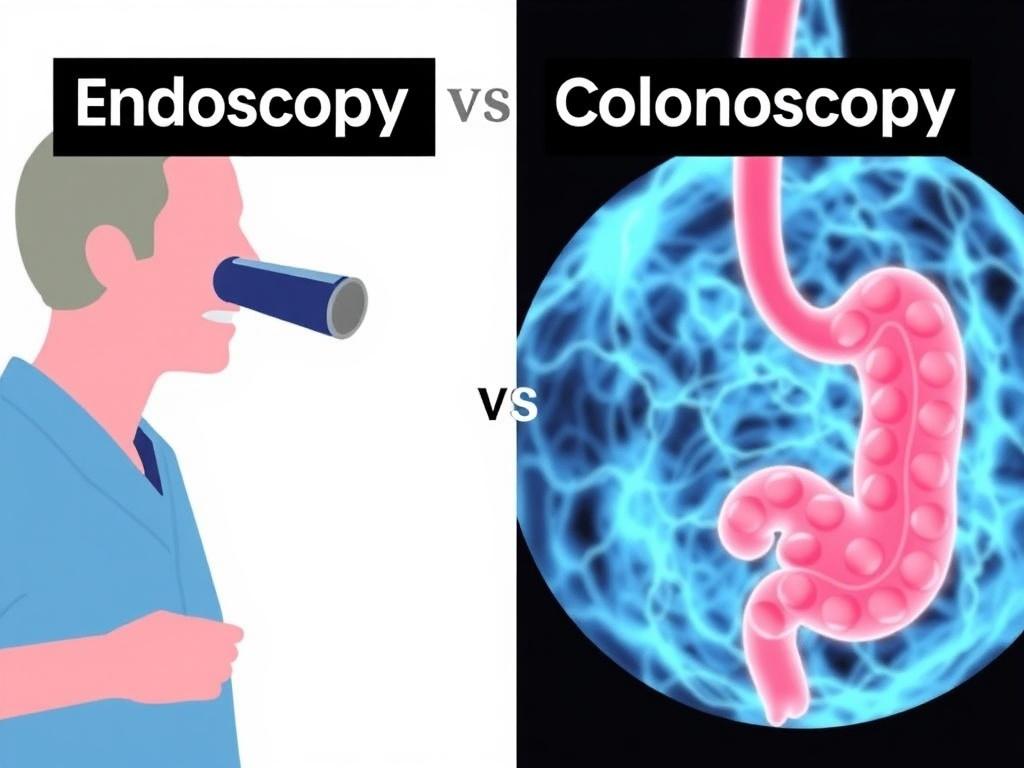
Endoscopy is an umbrella term that refers to using a flexible tube with a camera and light — called an endoscope — to look inside the body. In the context of the digestive system, endoscopy most often refers to upper endoscopy (also called esophagogastroduodenoscopy or EGD), which examines the esophagus, stomach and the first part of the small intestine (the duodenum). Upper endoscopies help diagnose causes of heartburn, bleeding, persistent nausea, difficulty swallowing and other upper-GI issues.
A colonoscopy, on the other hand, specifically examines the large intestine — the colon and the rectum — using a colonoscope, which is a similar flexible tube but designed for the lower digestive tract. Colonoscopies are commonly used for colorectal cancer screening, investigating causes of lower abdominal pain, rectal bleeding, or changes in bowel habits, and for removing polyps.
Both procedures use similar technology — a flexible tube, camera, and instruments for biopsies or removal — but they differ in the part of the digestive tract they explore, how patients prepare, and some aspects of risks and recovery.
How endoscopy and colonoscopy compare: a clear side‑by‑side
When you want to decide which procedure is appropriate, it’s helpful to see a direct comparison. Below is a practical table that highlights the main differences and similarities so you can spot what matters at a glance.
| Feature | Upper Endoscopy (EGD) | Colonoscopy |
|---|---|---|
| Area examined | Esophagus, stomach, duodenum | Entire colon (large intestine) and rectum |
| Purpose | Investigate upper GI symptoms; diagnose ulcers, gastritis, celiac disease, bleeding | Screening for colon cancer; remove polyps; evaluate lower GI bleeding or chronic diarrhea |
| Preparation | Fasting for several hours; stop certain meds per doctor | Bowel cleansing with laxatives; clear-liquid diet before procedure |
| Duration | 10–30 minutes typical | 20–60 minutes typical |
| Type of sedation | Conscious sedation or general in select cases | Conscious sedation or deeper sedation depending on setting |
| Biopsy or treatment | Biopsies, dilation, removal of small lesions | Polypectomy, biopsy, control of bleeding |
| Common risks | Perforation (rare), bleeding, reaction to sedation | Perforation (rare), bleeding after polypectomy, sedation issues |
| Recovery time | Short; often same day return to activities with caregiver help | Short; but need someone to drive you home and rest for remainder of day |
Why would a doctor recommend one over the other?
Doctors don’t choose procedures at random. The choice of endoscopy vs colonoscopy is driven by the symptoms, the part of the digestive tract suspected to be the problem, screening needs, and sometimes patient history such as previous findings or family history of disease.
If you’re experiencing upper abdominal pain, persistent heartburn, trouble swallowing, unexplained nausea and vomiting, or signs of upper-GI bleeding (like vomiting blood or black, tarry stools), an upper endoscopy is usually the test of choice. It allows the physician to directly visualize the lining of the esophagus and stomach, take biopsies to check for infection (like H. pylori) or celiac disease, dilate strictures, and treat bleeding sources.
If your concern is lower abdominal pain, rectal bleeding, significant changes in bowel habits, unexplained iron deficiency anemia, or you’re due for colorectal cancer screening, a colonoscopy is typically recommended. Colonoscopy is the gold standard for detecting colon polyps and early cancers and can remove polyps during the same procedure, which makes it both diagnostic and therapeutic.
Sometimes both are needed: for example, persistent, unexplained gastrointestinal symptoms that could originate in either the upper or lower tract, or when a full evaluation is required for conditions like inflammatory bowel disease.
Preparing for the procedures: what to expect at home
Preparation is one of the biggest differences between these procedures and often the most dreaded part for patients — especially the bowel prep for colonoscopy. Here’s what you should know about preparing for each.
- Upper endoscopy: You will be asked to fast — usually nothing to eat or drink for at least 6–8 hours prior. Your doctor will review medications and ask whether you take blood thinners, aspirin, diabetes medications, or supplements. Certain meds may need to be held. Plan for someone to drive you home if you receive sedation.
- Colonoscopy: Bowel prep involves a clear-liquid diet the day before and taking a prescribed laxative regimen to clean out the colon. Preparations vary (single-dose evening before, split-dose with some taken the morning of the procedure, etc.). The goal is a clean colon so the doctor can see clearly. Follow instructions closely — poor prep can mean rescheduling.
Preparation tips:
- Read and follow written instructions from your provider — they are created to minimize risks and maximize diagnostic value.
- Ask about your meds in advance — insulin, blood thinners, iron supplements, and herbal remedies may need special handling.
- Arrange transportation after the procedure if sedation will be used — driving is not allowed until sedatives wear off fully and your doctor clears you.
During the procedure: what happens step by step
Both procedures are usually performed in an outpatient endoscopy unit. Sedation practices vary, but most patients receive some form of sedation to be comfortable. Here’s a general step‑by‑step overview.
For upper endoscopy:
- You’ll change into a gown and meet the team. They’ll check your vital signs and review your medical history.
- A local anesthetic may be sprayed in your throat to reduce gagging; sedation is usually given intravenously.
- The endoscope is gently passed through your mouth and into the esophagus, stomach and duodenum while the physician watches a monitor.
- Biopsies or small interventions can be performed through the endoscope if needed.
- The scope is withdrawn and you recover in a monitoring area until sedation wears off.
For colonoscopy:
- Similar pre-procedure checks are done. IV sedation is typically administered.
- The colonoscope is inserted through the rectum and advanced through the colon; the camera sends images to a monitor.
- Air or CO2 is used to gently inflate the colon to improve visibility.
- Polyps can be removed, and biopsies taken. This is often done during the same procedure.
- After completion, the scope is withdrawn and you’re monitored during recovery.
Both procedures require careful teamwork from the physician, nurses, and anesthesiology staff (if involved). The doctor explains findings and gives post-procedure instructions before you go home.
Risks and complications: how common are they?
No medical procedure is without risk, but both endoscopy and colonoscopy are generally safe when performed by experienced teams. The most important complications to know about are:
- Perforation: A rare but serious tear in the lining of the organ. The risk is low — typically quoted as less than 1 in 1,000 for diagnostic colonoscopy and even lower for diagnostic upper endoscopy. The risk increases with therapeutic interventions like polypectomy.
- Bleeding: Can occur especially after biopsy or polyp removal. Most post-polypectomy bleeding is minor and controllable, but sometimes further treatment is needed.
- Reaction to sedation: Respiratory depression, changes in blood pressure, or allergic reactions are possible but uncommon; monitoring minimizes danger.
- Infection: Extremely rare in clean procedures but possible if interventions are performed.
Your doctor will review benefits and risks before you consent. If you notice severe abdominal pain, fever, heavy bleeding, shortness of breath, or other worrying symptoms after the procedure, contact your healthcare team right away.
Recovery and what to expect afterward
Recovery is fairly quick for both procedures, but there are practical differences.
For upper endoscopy:
- You might have a mild sore throat for a day or so from the scope.
- Because of sedation, you will need someone to take you home and you should rest for the remainder of the day.
- Most people can resume normal diet and activities the following day unless specific treatment was done that requires restrictions.
For colonoscopy:
- It is common to experience bloating or mild cramping due to the air used during the exam; passing gas relieves this.
- After polypectomy you may have small amounts of blood in the stool for a short time; contact the doctor if bleeding is heavy.
- Again, plan for a ride home and rest for the remainder of the day if sedated.
Both procedures: follow any specific instructions from your provider about diet, medications, and symptoms that should prompt urgent contact.
Screening and surveillance: when each test is used for prevention
Colonoscopy is the primary tool for colorectal cancer screening. For average-risk adults, many guidelines recommend starting screening at age 45 or 50 (depending on the guideline and country) and repeating intervals vary based on findings: every 10 years after a normal colonoscopy, sooner if polyps are found. During a colonoscopy, polyps can be removed before they become cancerous — this is screening and prevention in one.
Upper endoscopy is not a widespread screening tool for the general population but is used for targeted screening in people at high risk for certain conditions, such as those with Barrett’s esophagus (a precancerous condition related to chronic acid reflux), or in regions with high rates of stomach cancer. It’s more commonly used for diagnosis rather than mass screening in asymptomatic persons.
Surveillance intervals for both tests depend on findings. For example, if a colonoscopy finds high-risk polyps, the doctor may recommend a repeat colonoscopy in 3 years rather than the typical 10-year interval.
Cost, insurance, and access considerations
Cost and access vary by country, insurance plan, and medical system. In many places, screening colonoscopies are covered by insurance or public health programs up to certain ages because detecting and removing polyps prevents costly and deadly cancers. Diagnostic procedures (done for symptoms) may involve co-pays or different coverage rules.
Factors that affect cost:
- Facility fees (hospital or outpatient center)
- Physician and anesthesia fees
- Biopsy or polypectomy processing and pathology charges
- Pre-procedure testing if needed (blood tests, ECG)
If you are concerned about cost, contact your insurer and the facility ahead of time to ask about coverage, preauthorization, and what portions you might be responsible for. Many centers also offer financial counseling.
Common myths and fears — let’s clear them up
Fear of scopes, embarrassment, and worry about the prep are common. Here are some myths and realities to help you feel better prepared.
- Myth: “You’ll be wide awake the whole time and feel everything.” Reality: Sedation makes many people drowsy and comfortable; the procedure is generally painless.
- Myth: “Bowel prep is unbearable.” Reality: It’s uncomfortable, but modern preps and split-dose strategies make them tolerable. Following instructions makes the difference between a successful exam and a rescheduled one.
- Myth: “If I feel fine, I don’t need screening.” Reality: Polyps and early-stage cancers can be symptomless. Screening is about prevention and catching disease early.
- Myth: “A colonoscopy always involves surgery.” Reality: Colonoscopy is minimally invasive; polyps removed are treated through the scope, not open surgery.
When both tests might be needed
There are clinical situations where both upper endoscopy and colonoscopy are performed as part of a comprehensive evaluation. Examples include:
- Unexplained gastrointestinal bleeding where the source isn’t obvious from symptoms.
- Iron deficiency anemia when both upper and lower GI sources are possible.
- Inflammatory bowel disease workup, where the doctor wants to view both the upper and lower GI tracts to assess disease extent.
- Preoperative assessment for certain conditions or when symptoms span the entire digestive tract.
Sometimes both tests are coordinated closely, either the same day or on separate days, depending on logistics, the need for bowel prep, and patient preference.
Biopsies and polyp removal: what can be treated during the test
One of the major advantages of these procedures is that diagnosis and some treatments can occur in one visit. During an upper endoscopy, tiny instruments can take tissue samples (biopsies) to investigate inflammation, infection, H. pylori, or celiac disease. Small lesions can sometimes be removed or dilated.
During colonoscopy, polyps are routinely removed (polypectomy) with snares or forceps and sent to pathology. Removing polyps reduces the risk of colorectal cancer and is one of the main reasons colonoscopy is so valuable. Larger or more complex polyps may require specialized techniques or referral to an advanced endoscopist.
Ask your doctor whether biopsies or polypectomy are planned and what the implications are for recovery and follow-up.
Sedation: options and safety
Sedation practices vary by region and patient needs. Options include:
- Minimal sedation (anxiolysis) — patient is relaxed but fully conscious.
- Moderate (conscious) sedation — patient is drowsy and may have little memory of the procedure.
- Deep sedation or general anesthesia — deeper unconsciousness, typically used for certain patients or based on facility practices.
Sedation is generally safe when administered and monitored by trained staff. Tell your team about sleep apnea, heart or lung disease, and all medications you take, as these can affect sedation choices. Post-procedure you’ll need someone to drive you home if sedated, and you should avoid important decisions, work, or driving for the rest of the day.
Pediatric and special population considerations
Children often undergo endoscopy or colonoscopy for different reasons than adults: growth problems, severe abdominal pain, persistent vomiting, failures to thrive, unexplained bleeding, or suspected inflammatory bowel disease. Pediatric procedures are typically performed with age-appropriate anesthesia and equipment in specialized pediatric units.
Older adults may have higher risks due to medical comorbidities, so pre-procedure evaluation and tailored sedation plans are important. Pregnancy is a special situation: urgent endoscopic procedures can be done if necessary, but elective procedures are often postponed until after delivery.
Alternatives to endoscopy and colonoscopy

In some situations, less invasive or complementary tests are available:
- CT colonography (virtual colonoscopy) — imaging test that looks at the colon but does not allow for polyp removal; abnormal findings still require colonoscopy.
- Stool-based tests — FIT (fecal immunochemical test) or Cologuard detect blood or DNA markers associated with cancer and may be used for screening; positive tests require diagnostic colonoscopy.
- Barium swallow or upper GI series — older imaging tests that can show structural problems but aren’t as sensitive as endoscopy for mucosal disease.
- Capsule endoscopy — swallowing a camera pill can visualize the small intestine, useful when other tests don’t show a source of bleeding; it does not allow biopsies or interventions.
These alternatives have roles but often cannot replace the therapeutic ability of traditional endoscopy and colonoscopy.
How to choose the right test: questions to ask your doctor
Deciding which procedure is appropriate should involve clear communication with your physician. Useful questions include:
- Which test do you recommend and why?
- What are the benefits and risks specifically for my situation?
- How should I prepare, and what medications should I stop or continue?
- What type of sedation will you use?
- Can any findings be treated during the procedure?
- How will I get the results and what follow-up should I expect?
- What happens if the bowel prep is poor or the exam is incomplete?
A good conversation will leave you informed and comfortable with the plan.
Frequently asked questions (FAQs)
Will the procedure be painful?
Both procedures are usually well tolerated with sedation. Many patients report little or no pain and may remember little about the experience.
How long will the results take?
Immediate visual findings are often discussed right after the procedure. Biopsy or pathology results typically take several days to a week depending on the test and lab.
Can you eat after an upper endoscopy?
Often yes, once the gag reflex returns and your doctor is sure there are no restrictions. You may start with liquids and progress to solids as tolerated.
How often do I need repeat colonoscopy?
It depends on findings. With a normal exam, many people return in 10 years for screening. If polyps are found, surveillance intervals may be 3–5 years or more frequent based on risk.
Practical tips to make the experience easier

Preparing mentally and practically can reduce anxiety and improve the experience:
- Follow preparation instructions carefully — especially bowel prep — to avoid rescheduling.
- Bring a list of medications, allergies, and a support person to take you home if sedated.
- Wear comfortable clothing and avoid jewelry.
- Have a bland meal plan for after the procedure in case you feel off that day.
- Write down questions before your appointment so you don’t forget them when you’re nervous.
The future of endoscopic procedures: less invasive, more powerful

Endoscopy and colonoscopy continue to evolve. Advances include high-definition imaging, chromoendoscopy and narrow-band imaging to better detect subtle lesions, improvements in sedation safety, and advanced therapeutic techniques that allow removal of very large polyps endoscopically instead of surgery. Capsule endoscopy, motorized capsule technology, and artificial intelligence to assist detection are promising developments aimed at making exams more accurate and patient-friendly.
Conclusion
Endoscopy and colonoscopy are powerful, related tools that let doctors see and treat many problems of the digestive tract; the key difference is the part of the GI tract each examines — upper endoscopy looks at the esophagus and stomach, while colonoscopy inspects the colon and rectum — and that colonoscopy plays a central role in colorectal cancer screening because it allows polyp removal; both procedures are generally safe, require specific preparation (with bowel prep being the most involved for colonoscopy), and are often done under sedation with quick recovery, and deciding which test you need depends on symptoms, screening needs, and shared decision-making with your physician.
Читайте далее: