<diverticulitis is a condition that affects millions of people worldwide, yet many aren’t fully aware of what it entails. If you’ve ever experienced unexplained abdominal pain or digestive discomfort, understanding diverticulitis might be crucial to your health. This article dives deep into diverticulitis, shedding light on its symptoms, causes, and treatment options in a way that’s easy to understand and engaging to read. By the end of this exploration, you’ll have a clear idea of how to recognize diverticulitis and what steps to take if you suspect you might be dealing with this condition.
What Is Diverticulitis?
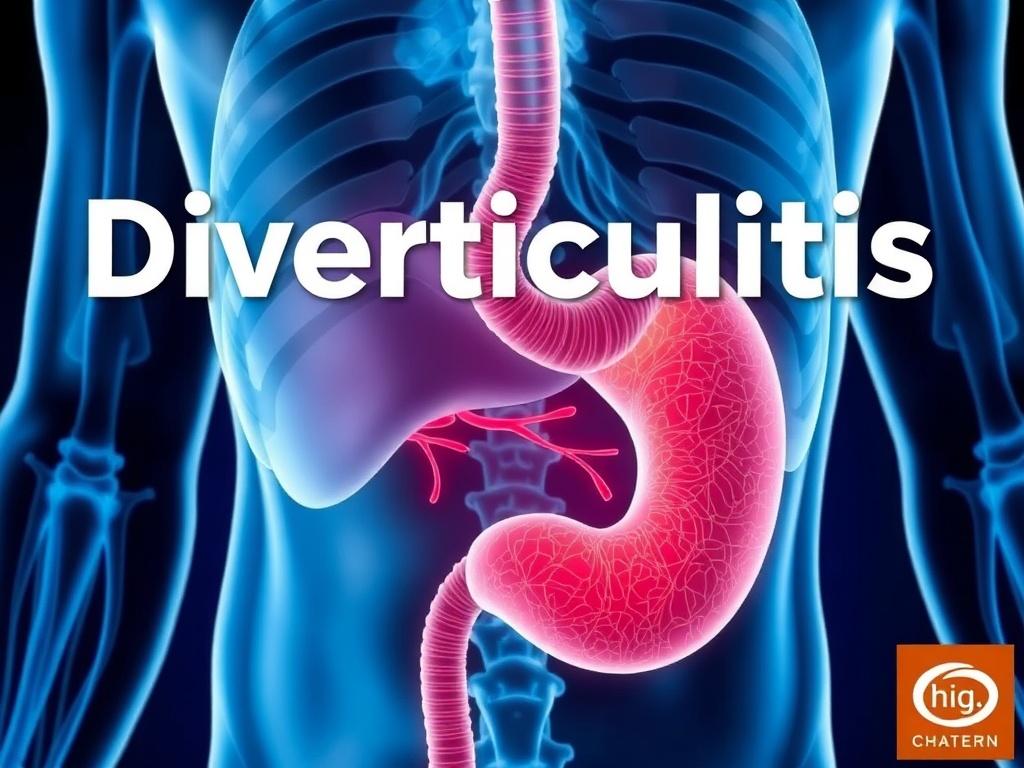
Diverticulitis occurs when small, bulging pouches called diverticula, which develop in the lining of the digestive system, become inflamed or infected. These pouches are most commonly found in the large intestine, particularly in the lower part called the sigmoid colon. While having diverticula alone (a condition called diverticulosis) might not cause symptoms, the progression to diverticulitis involves swelling and infection, which often leads to discomfort and other complications.
Diverticulitis can vary from mild to severe, depending on the level of inflammation and whether any complications arise, such as abscesses or perforations in the colon. The good news is many people with diverticulitis can manage it successfully with appropriate care and lifestyle adjustments.
Symptoms of Diverticulitis
Recognizing the symptoms of diverticulitis early is essential for timely treatment. Often, people ignore mild symptoms, thinking they might be related to food or minor digestive issues, but persistent signs should never be overlooked.
Common Symptoms
- Abdominal pain: The most frequent symptom, usually felt on the lower left side of the abdomen.
- Fever: A sign your body is fighting infection.
- Nausea and vomiting: Sometimes accompany the abdominal pain.
- Constipation or diarrhea: Changes in bowel habits often occur during an episode.
- Abdominal tenderness: The area may feel sore to touch.
- Bloody stools: Though less common, bleeding can happen if diverticula bleed.
In more severe cases, diverticulitis symptoms may include severe cramping, chills, and even signs of infection spreading beyond the colon, requiring immediate medical attention.
Symptoms Table
| Symptom | Description | Commonality |
|---|---|---|
| Abdominal pain | Pain usually located in the lower-left abdomen | Very common |
| Fever | Elevated body temperature indicating infection | Common |
| Nausea and vomiting | Feeling sick or actual vomiting episodes | Common |
| Changes in bowel habits | Constipation or diarrhea | Common |
| Bloody stools | Blood visible in bowel movements | Less common |
What Causes Diverticulitis?

The exact cause of diverticulitis isn’t always straightforward, but several factors can contribute to the development of diverticula and their subsequent inflammation. Understanding these causes can help in both prevention and management.
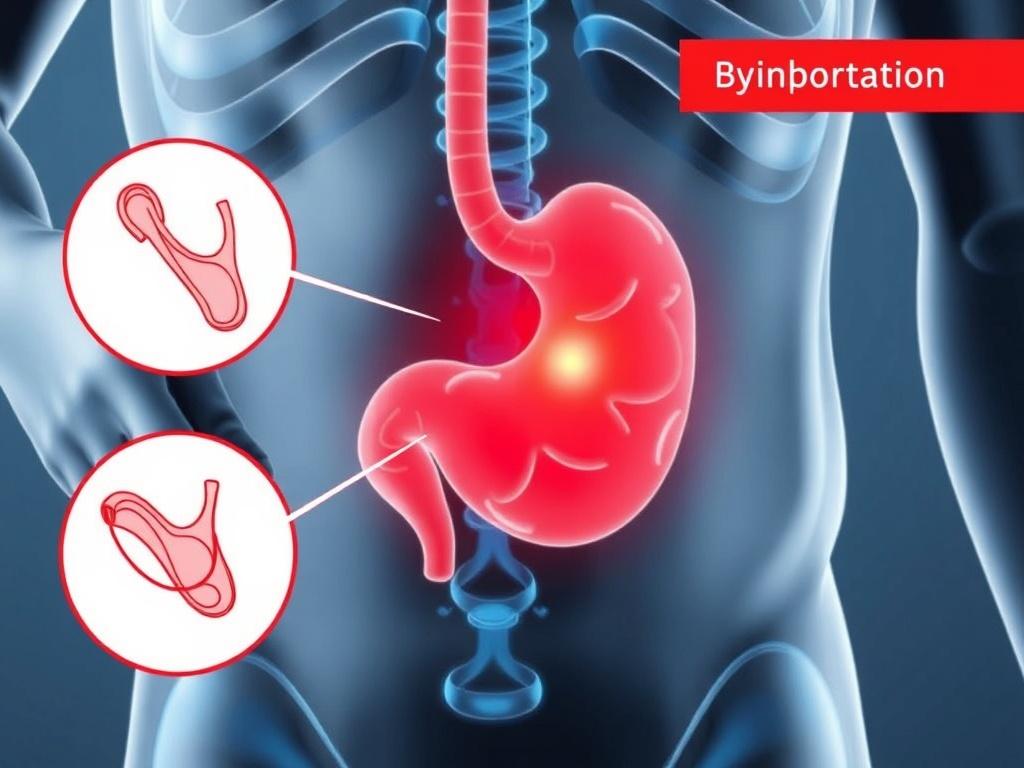
The Role of Diverticulosis
Most people with diverticulitis first had diverticulosis, which means they had diverticula present in the colon without inflammation. Diverticulosis is fairly common, especially as people age, and is often linked to diet and lifestyle habits.
Main Causes and Risk Factors
- Low-fiber diet: Diets low in fiber can cause constipation and increased pressure in the colon, contributing to the formation of diverticula.
- Aging: Diverticula tend to develop as people get older, especially after 40 or 50 years of age.
- Chronic constipation: Straining during bowel movements increases pressure on the colon walls.
- Obesity: Excess weight has been linked to a higher risk of developing diverticulitis.
- Smoking: Tobacco use can increase risk and severity.
- Lack of exercise: A sedentary lifestyle contributes to poor bowel health.
- Certain medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), steroids, and opioids can increase the risk.
How Diverticulitis Develops
When fecal matter or bacteria become trapped in the diverticula, they can cause irritation and infection leading to diverticulitis. This infection triggers inflammation, which causes the typical symptoms such as pain and fever.
Diagnosing Diverticulitis

If you or someone you know shows symptoms of diverticulitis, a healthcare professional will perform tests to confirm the diagnosis and determine the severity. Early diagnosis is key to avoiding complications and starting appropriate treatment.
Diagnostic Tools
- Physical examination: Checking for abdominal tenderness and other signs.
- Blood tests: Looking for signs of infection, like elevated white blood cells.
- CT scan: The most common and effective imaging test to see inflammation or abscesses.
- Colonoscopy: Sometimes recommended after initial treatment to rule out other causes.
- Ultrasound: Alternative imaging depending on case and availability.
Treatment Options for Diverticulitis

Treatment for diverticulitis depends on the severity of the condition. Mild cases can often be managed at home, while severe infections might require hospitalization or even surgery.
Home and Medical Treatments
- Antibiotics: Prescribed if infection is confirmed or highly suspected.
- Diet modification: Starting with clear liquids and gradually returning to a high-fiber diet.
- Pain management: Over-the-counter pain relievers and sometimes prescription medications.
- Rest: Allowing the colon to heal by avoiding strenuous activities temporarily.
When Surgery Is Needed
In cases where diverticulitis leads to complications such as abscesses, perforations, or persistent symptoms despite treatment, surgery may be necessary. Surgical options vary depending on the situation:
- Bowel resection: Removing the affected section of the colon.
- Drainage: Draining abscesses if present.
- Temporary colostomy: Sometimes performed to allow the colon to heal.
Long-Term Management and Prevention
After recovering from an episode of diverticulitis, it’s essential to adopt habits that reduce the risk of recurrence:
- Increase fiber intake: Fruits, vegetables, whole grains, and legumes.
- Stay hydrated: Drinking plenty of water helps prevent constipation.
- Exercise regularly: Physical activity supports bowel health.
- Avoid smoking and reduce alcohol: Both can contribute to digestive issues.
Comparing Diverticulitis to Other Digestive Conditions

It’s easy to confuse diverticulitis with other digestive disorders because many share similar symptoms. Here’s a quick comparison to help clarify:
| Condition | Symptoms | Typical Causes | Treatment |
|---|---|---|---|
| Diverticulitis | Lower-left abdominal pain, fever, nausea | Inflammation of diverticula | Antibiotics, diet changes, sometimes surgery |
| Irritable Bowel Syndrome (IBS) | Abdominal pain, bloating, diarrhea or constipation | Unknown, often stress-related | Diet management, stress reduction |
| Appendicitis | Lower-right abdominal pain, fever, nausea | Inflammation of appendix | Surgical removal of appendix |
| Inflammatory Bowel Disease (IBD) | Chronic diarrhea, abdominal pain, weight loss | Autoimmune inflammation | Medication, sometimes surgery |
Living with Diverticulitis: Tips for Daily Life

Managing diverticulitis goes beyond treating acute episodes. Many people lead full, active lives while managing this condition by making smart lifestyle choices and understanding their body’s signals.
Daily Tips to Stay Comfortable and Healthy
- Monitor your diet: Keep track of what foods trigger symptoms and focus on a high-fiber regimen.
- Stay active: Regular physical activity can improve digestion and reduce constipation.
- Stay hydrated: Drinking enough water softens stools and eases bowel movements.
- Manage stress: Stress can impact digestion, so incorporating relaxation methods like meditation or yoga can be beneficial.
- Regular check-ups: Seeing your healthcare provider ensures any changes are promptly addressed.
Foods to Include and Avoid
| Foods to Include | Foods to Avoid |
|---|---|
| Whole grains (brown rice, oats) | Processed foods high in fat and sugar |
| Fresh fruits and vegetables | Red meat and high-fat dairy |
| Legumes (beans, lentils) | Seeds and nuts (depending on tolerance) |
| Plenty of water | Alcohol and caffeine in excess |
When to See a Doctor
Knowing when to seek medical advice is crucial. If you experience sudden severe abdominal pain, persistent fever, vomiting, or bloody stools, you should contact your healthcare provider immediately. Early intervention can prevent serious complications and ensure the best outcome for diverticulitis.
Frequently Asked Questions About Diverticulitis

Can diverticulitis be cured?
There is no permanent cure for diverticulosis or diverticulitis, but episodes can be treated and prevented by managing symptoms and lifestyle factors.
Is diverticulitis contagious?
No, it is not contagious. Diverticulitis results from inflammation or infection in the digestive tract, not from exposure to others.
Can I exercise with diverticulitis?
During a flare-up, it is best to rest. Once symptoms improve, moderate exercise is encouraged to maintain digestive health.
Should I avoid nuts and seeds?
While traditionally advised to avoid nuts and seeds, recent studies suggest they may not increase risk. However, personal tolerance varies.
How long does recovery take?
Mild cases often improve within a week with proper treatment; severe cases may require longer recovery and potentially surgery.
Wrapping Up

Diverticulitis is a common but potentially serious digestive condition that affects many adults worldwide. Understanding its symptoms, causes, and treatment options empowers you to take control of your digestive health. Recognizing the signs early, seeking timely medical care, and making wise lifestyle choices can make a significant difference in managing diverticulitis effectively. Whether you’re currently dealing with diverticulitis or simply want to be informed, this knowledge equips you for better health and confidence in your daily life.
Читайте далее: