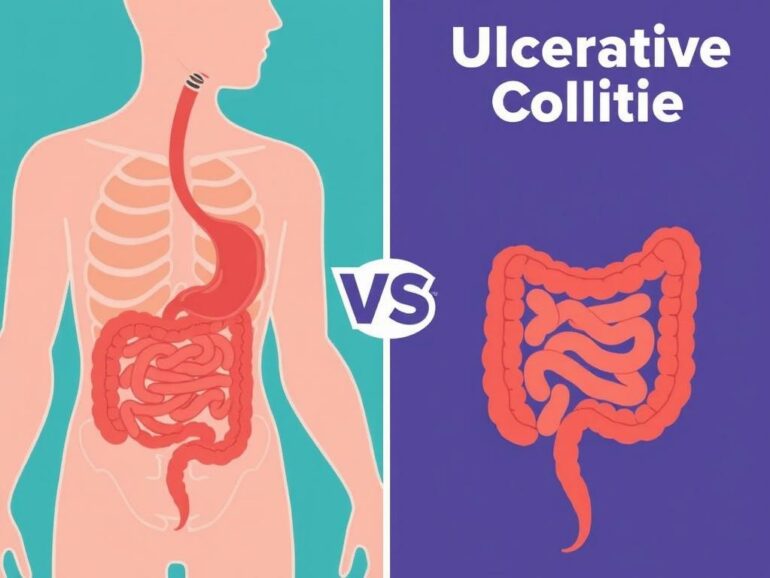
When it comes to chronic inflammatory conditions affecting the digestive tract, Crohn’s disease and ulcerative colitis often come up in conversation. Both fall under the category of inflammatory bowel disease (IBD), but despite some overlapping symptoms, they are distinct disorders with their own unique characteristics. If you or someone you know has recently been diagnosed or is trying to understand what sets these two conditions apart, you’re not alone. Understanding the differences between Crohn’s disease vs. ulcerative colitis can help patients, caregivers, and friends manage the conditions more effectively and navigate treatment options with greater confidence.
In this article, we’ll take a detailed look at Crohn’s disease and ulcerative colitis from what causes them, how they present, diagnostic approaches, treatment strategies, and long-term outlooks. By the end, you’ll have a clearer picture of each disease’s nature and learn how to cope better with daily life when managing IBD.
What is Crohn’s Disease?

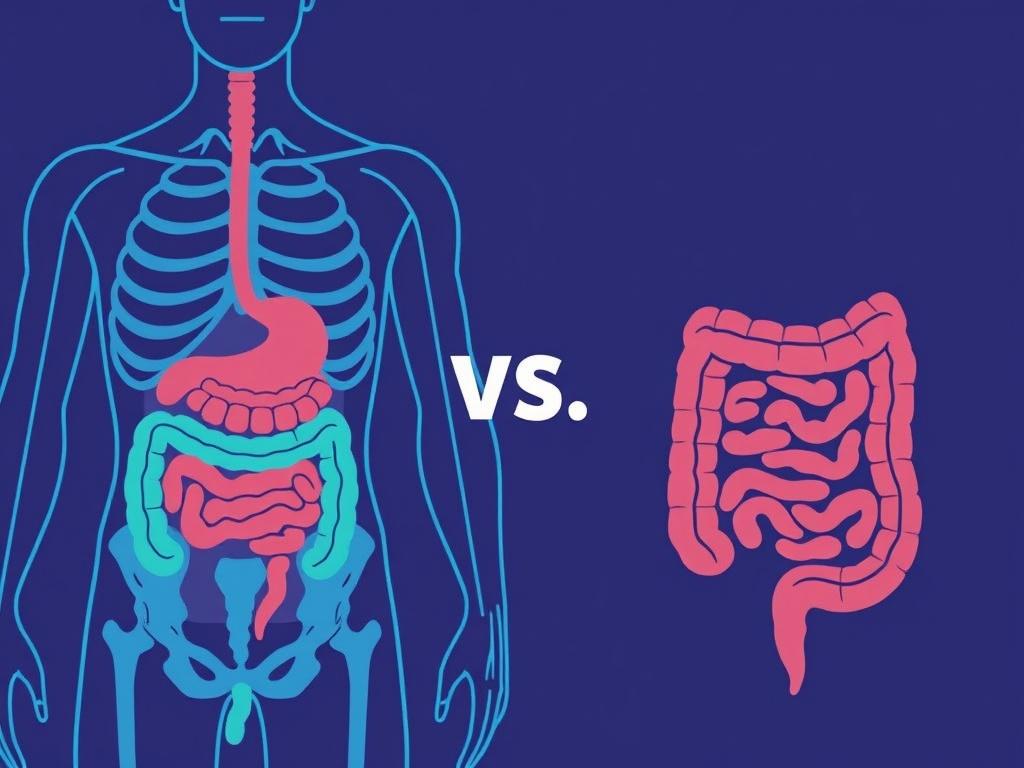
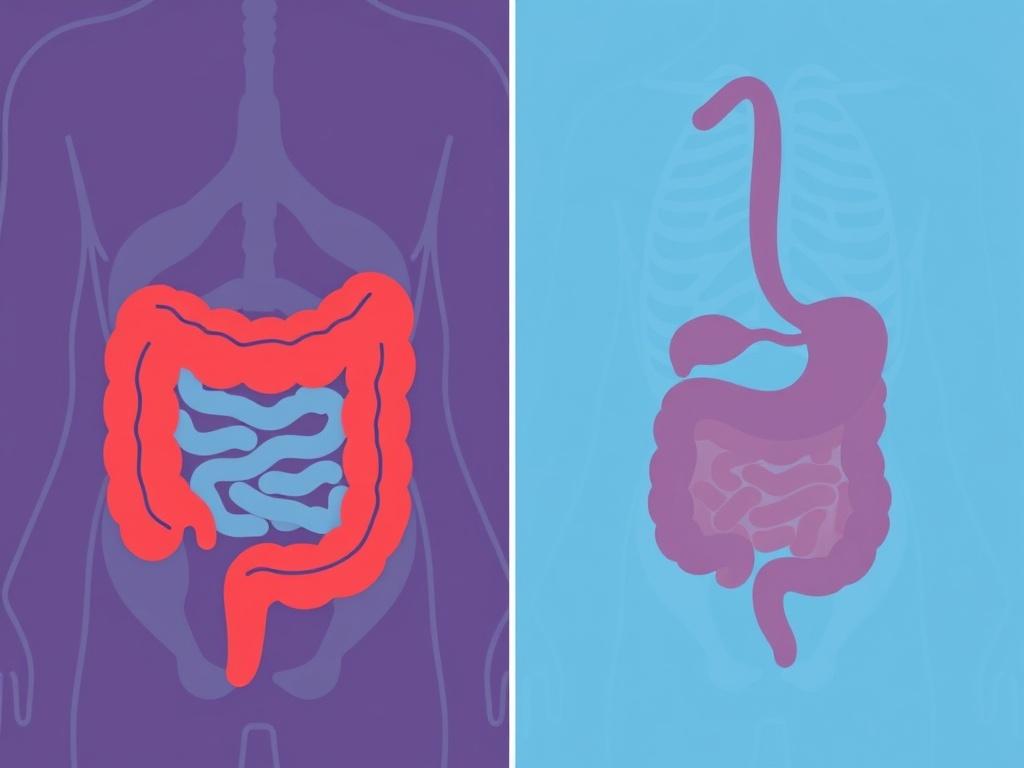
Crohn’s disease is a type of chronic inflammatory bowel disease that can affect any part of the gastrointestinal tract, from the mouth all the way to the anus. Although it can impact any section, the most common areas involved are the small intestine, especially the terminal ileum, and the colon. The inflammation caused by Crohn’s disease can penetrate deep into the layers of the bowel walls, which can lead to complications such as strictures (narrowing of the intestines), fistulas (abnormal connections between organs), and abscesses.
The exact cause of Crohn’s disease is not fully understood, but it is believed to be a mix of genetic susceptibility, environmental factors, and an abnormal immune response. The immune system mistakenly attacks the intestinal tract, leading to chronic inflammation. Symptoms often develop gradually and may vary over time, depending on the location and severity of the inflammation.
Common Symptoms of Crohn’s Disease
- Persistent diarrhea
- Abdominal pain and cramping
- Weight loss and reduced appetite
- Fatigue and malaise
- Fever
- Sometimes blood in the stool
- Extraintestinal symptoms such as joint pain, skin rashes, or eye inflammation
Because Crohn’s disease can affect different sections of the bowel, symptoms can be quite diverse. Some patients may experience severe abdominal pain or complications like bowel obstruction, while others might only have mild discomfort and intermittent diarrhea.
What is Ulcerative Colitis?
Ulcerative colitis (UC) is another inflammatory bowel disease, but unlike Crohn’s disease, it is limited exclusively to the colon (large intestine) and the rectum. The inflammation in ulcerative colitis affects only the innermost lining of the colon, which is why complications such as strictures and fistulas are less common compared to Crohn’s. The inflammation in UC usually starts at the rectum and spreads continuously throughout the colon.
The cause of ulcerative colitis, like Crohn’s, involves genetic, immune, and environmental factors. The immune system’s improper reaction causes the colon’s lining to become inflamed, ulcerated, and bleed. This results in symptoms that can fluctuate in severity, ranging from mild discomfort to severe frequent bloody diarrhea.
Common Symptoms of Ulcerative Colitis
- Abdominal pain and cramping, often on the left side
- Urgent and frequent diarrhea with blood and mucus
- Rectal bleeding
- Weight loss
- Fatigue
- Fever during flare-ups
- Extraintestinal manifestations like arthritis or skin problems
Ulcerative colitis symptoms typically come and go in flare-ups, during which inflammation worsens. In between flare-ups, patients might feel relatively symptom-free.
Crohn’s Disease vs. Ulcerative Colitis: A Side-by-Side Comparison
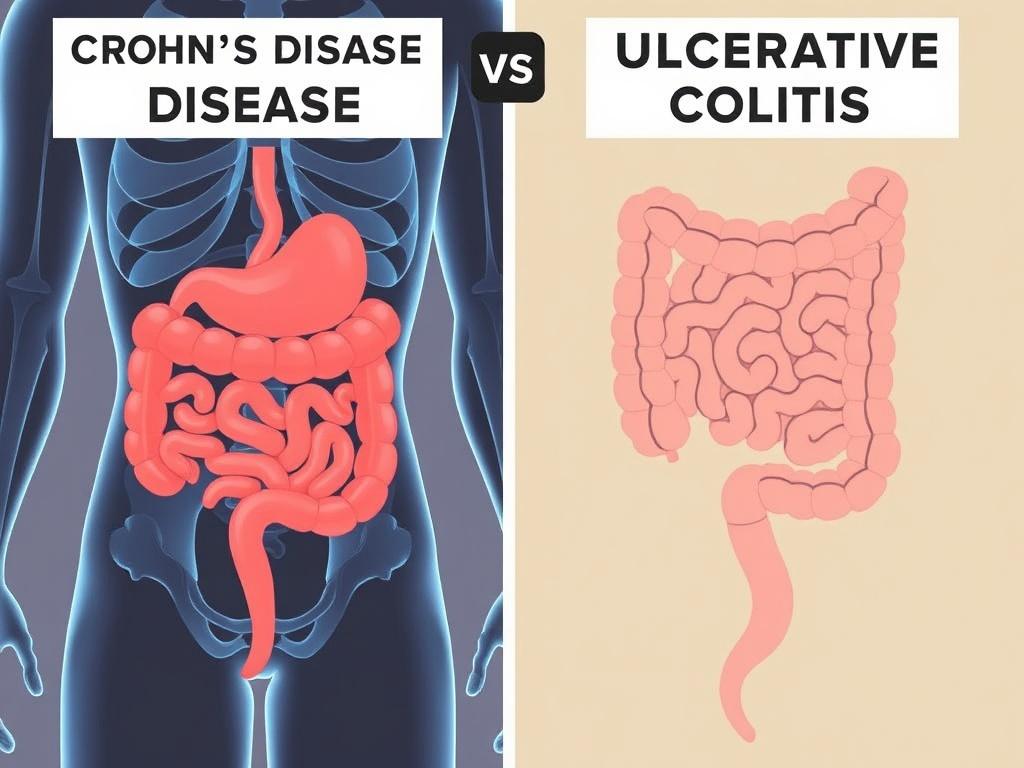
To better understand the differences between Crohn’s disease and ulcerative colitis, it is helpful to look at their unique and overlapping characteristics in a side-by-side table. This comparison covers key aspects like affected regions, depth of inflammation, common symptoms, and complications.
| Feature | Crohn’s Disease | Ulcerative Colitis |
|---|---|---|
| Location of Inflammation | Any part of the GI tract (mouth to anus); often terminal ileum and colon | Colon and rectum only; inflammation continuous starting at rectum |
| Depth of Inflammation | Full thickness (all layers) of intestinal wall | Superficial (mucosal lining only) |
| Pattern of Inflammation | Patchy, with healthy segments between inflamed areas (skip lesions) | Continuous inflammation |
| Common Symptoms | Diarrhea, abdominal pain, weight loss, fatigue, sometimes blood in stool | Bloody diarrhea, abdominal pain, urgency, weight loss, fatigue |
| Complications | Strictures, fistulas, abscesses, malnutrition | Colon perforation, severe bleeding, toxic megacolon |
| Risk of Colon Cancer | Increased if colon involved | Higher risk with longer disease duration |
| Surgery | May not cure; often needed for complications | Can be curative if colon removed |
Causes and Risk Factors
Both Crohn’s disease and ulcerative colitis arise from complex interactions of genetics, immune dysfunction, and environmental exposures. Here’s a closer look at these components:
Genetics
Having a family member with IBD increases your risk for developing either Crohn’s disease or ulcerative colitis. Specific genes like NOD2/CARD15 are linked more closely to Crohn’s, while other gene variations can predispose to ulcerative colitis. Still, genetics alone do not cause these diseases; they increase susceptibility.
Immune System Dysfunction
The immune system plays a key role in both conditions. In IBD, the immune system mistakenly attacks cells in the gut lining, causing chronic inflammation. This abnormal response leads to tissue damage and symptoms. Researchers are exploring how gut bacteria, immune cells, and environmental triggers contribute to this process.
Environmental Factors
Several environmental factors may increase someone’s risk of IBD, including:
- Smoking: Particularly increases risk and severity of Crohn’s disease but may have a protective effect in ulcerative colitis.
- Diet: While no specific food causes IBD, processed foods and high fat intake may contribute.
- Infections: Past gastrointestinal infections might trigger IBD in susceptible individuals.
- Use of nonsteroidal anti-inflammatory drugs (NSAIDs): These can sometimes worsen symptoms.
How Are Crohn’s Disease and Ulcerative Colitis Diagnosed?
Correct diagnosis is essential for effective management. Doctors use a combination of clinical evaluation, laboratory tests, imaging, and endoscopic procedures to differentiate Crohn’s disease vs. ulcerative colitis.
Medical History and Physical Exam
The physician will inquire about symptom patterns, family history, medication use, and perform a physical exam, often including an abdominal and rectal exam.
Laboratory Tests
- Blood tests to check for anemia, inflammation markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), and signs of infection.
- Stool tests to rule out infections and check for inflammation markers such as calprotectin and lactoferrin.
Endoscopy and Biopsy
Colonoscopy is the gold standard in diagnosing and distinguishing between Crohn’s disease and ulcerative colitis. It allows direct visualization of inflammation, mucosal ulcers, and the pattern of affected areas. Biopsy samples are taken from inflamed tissue to find microscopic characteristics and rule out other conditions.
Imaging Studies
- CT scans and MRI, especially MR enterography, can evaluate deeper layers of the bowel wall and detect complications like fistulas or abscesses.
- Small bowel follow-through x-rays can help identify Crohn’s disease involvement beyond the colon.
Treatment Options for Crohn’s Disease and Ulcerative Colitis
Though both diseases share inflammation as a common theme, treatment approaches must be tailored to their specific characteristics and severity.
Medications
The goal of treatment is to reduce inflammation, induce and maintain remission, manage symptoms, and prevent complications.
- Aminosalicylates (5-ASA): Often used in mild to moderate ulcerative colitis but less effective in Crohn’s disease.
- Corticosteroids: Effective for short-term relief during flare-ups but not recommended for long-term use due to side effects.
- Immunomodulators: Drugs like azathioprine or methotrexate help suppress the immune response.
- Biologics: These newer targeted therapies, such as anti-TNF agents (infliximab, adalimumab), vedolizumab, and ustekinumab, can control moderate to severe disease and complications.
- Antibiotics: Sometimes used in Crohn’s disease for infections or fistulas.
Surgery
While medication is the primary treatment, surgery plays different roles based on the disease.
- Crohn’s Disease: Surgery is not curative but used to remove damaged sections of the intestine, treat strictures, fistulas, or abscesses. Recurrence after surgery is common.
- Ulcerative Colitis: Surgery involves removing the entire colon and rectum (proctocolectomy), which can essentially cure the disease as it is limited to the colon.
Lifestyle and Dietary Management
While no specific diet cures IBD, patients often benefit from working with dietitians to manage symptoms and maintain nutrition. Some tips include:
- Eating smaller, frequent meals
- Avoiding high-fiber foods during flare-ups
- Limiting fatty or spicy foods if they worsen symptoms
- Staying hydrated
- Considering vitamin and mineral supplements to address deficiencies
Extraintestinal Symptoms and Impact on Quality of Life
It’s important to remember that both Crohn’s disease and ulcerative colitis can affect more than just the intestines. Around 25–40% of patients experience extraintestinal manifestations involving joints, skin, eyes, and liver. These might include:
- Arthritis and joint pain
- Erythema nodosum (a painful skin rash)
- Uveitis or other eye inflammations
- Primary sclerosing cholangitis (liver disease)
Living with chronic illness challenges mental health as well. Anxiety, depression, and social isolation can accompany IBD, making holistic care that addresses physical and emotional well-being essential.
Monitoring, Prognosis, and Long-Term Care
After diagnosis, ongoing monitoring is crucial to assess disease activity, adjust treatments, and screen for complications such as colorectal cancer, which has increased risk particularly in ulcerative colitis and longstanding Crohn’s disease affecting the colon.
Periodic colonoscopies, blood tests, and imaging studies form part of routine care. With advances in treatment, many patients can achieve long-term remission and lead productive lives. However, there is currently no cure, highlighting the importance of early diagnosis, tailored therapy, and supportive care.
Summary Table: Crohn’s Disease vs. Ulcerative Colitis at a Glance
| Aspect | Crohn’s Disease | Ulcerative Colitis |
|---|---|---|
| Affected Areas | Any GI tract section; patchy involvement | Colon and rectum; continuous inflammation |
| Inflammation Depth | Transmural (all layers) | Mucosal (inner lining) |
| Common Symptoms | Abdominal pain, diarrhea, fatigue, weight loss | Bloody diarrhea, abdominal cramps, urgency |
| Complications | Strictures, fistulas, abscesses | Toxic megacolon, severe bleeding |
| Treatment | Medications, surgery for complications | Medications, curative surgery possible |
| Risk of Colon Cancer | Increased with colon involvement | Higher with longer disease duration |
When to See a Doctor
Both conditions can lead to serious complications if left untreated. Immediate medical attention is needed for symptoms such as severe abdominal pain, persistent vomiting, high fever, blood loss, or signs of intestinal blockage.
Support and Resources
Connecting with IBD support groups, patient advocacy organizations, and counseling services can help manage the emotional toll and provide practical advice on living well with Crohn’s disease or ulcerative colitis.
Conclusion
Understanding the difference between Crohn’s disease vs. ulcerative colitis is key for effective management of these chronic inflammatory bowel conditions. While both share symptoms and immune-driven inflammation, they differ in where and how the digestive tract is affected, their patterns of inflammation, potential complications, and approaches to treatment. Crohn’s disease can involve the entire gastrointestinal tract and involves deeper tissue layers, often requiring surgery for complication management but not cure. Ulcerative colitis is confined to the colon’s inner lining, making surgical removal of the colon a potential cure. The complexity of IBD means personalized care, lifestyle adjustments, and ongoing monitoring are essential. With growing advances in medical treatments and supportive care, individuals with Crohn’s disease or ulcerative colitis can aspire to improved symptom control, better quality of life, and hope for the future. If you’re navigating these conditions, working closely with your healthcare team and seeking support can make all the difference on this challenging journey.
Читайте далее: